Live your best to life’s end.
There’s still lots of life to live–whatever health and medical decisions that may be ahead. For many, feeling ‘alive’ right to the end means feeling useful for as long as possible. For others, it’s peace of mind that brings a peaceful end. For most, it’s feeling wanted, valued, respected and listened-to that are all-important. The pleasures of everyday life can be just as meaningful: what makes you smile, what brings you happiness and joy and what gives you comfort.
It’s often that small stuff that can make a big difference: There are creative ways to accomplish what may seem out of reach – like the man on the rock who may not be able to be physically near an ocean, but may be able to turn to technology to inspire a solution. Paying attention to small pleasures shifts the focus from ‘what I don’t want at life’s end’ to ‘what will make a positive difference to me at life’s end.’ It’s an approach with its own reward: helping someone have the best end can help everyone involved.
Need Inspiration?
How would you fill in the blank? Check out whiteboards and 60-second BestEndings videos: instagram @MyBestEndings
Need Information?
It can be a long road to learning about and planning for the best end-of-life experience. There’s lots to consider and emotions to tackle. Pick your own starting points: personal or medical decisions or specific topics. You can come back for more and then document your end of life wishes
Caring for aging parents: Chronic illness
Heart and kidney failure, frailty, Alzheimer’s, Lung Disease, Diabetes
Palliative Comfort Care and Quality of Life
The Palliative and Hospice approach: comfort and quality of life is what it’s all about
Understanding Medical Terms and Jargon
Cardio Pulmonary Resuscitation: CPR, Do Not Resuscitate: DNR, Allow Natural Death: A.N.D
Traditions, Culture and Being Remembered
Time honored customs can help at life’s end, ways to keep memories alive.
Modern Medicine can keep you alive
End of life: grief and bereavement
Knowing what End of Life looks like can ease the process; often grief starts long before the end.
Decision-Makers: Consent and Conflict
Surrogate, Substitute, Agent, Proxy: who will make sure your end of life wishes are followed.
Advance Directives, Living Will, End of Life Wishes
Create your own end of life, Advance Directives Living Will with an interactive form

Medical Aid in Dying: I signed up to be a witness
I was nervous about this new role I’d signed up for: volunteering to be one of two witnesses to make official a patient’s request for medical assistance in dying.This involves witnessing the paperwork necessary for a MAID (Medical Aid in Dying) request. The...

Live in memory, Live in love
This is Sam, my father-in-law. He's going into his 103 year, and is still smiling. Yet every night, his last words before falling asleep: God, please let me die He's not suffering in any major way: the swollen ankles and chronically congested chest don't bother him...
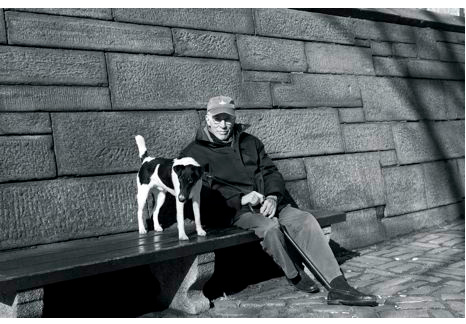
Men writing about The End of Life
Men writing from the inside out about life’s end. In the picture in The New Yorker, sitting with his dog, on a bench by a park, Roger Agnell, looks none of his 93 years. Famous for his sports writing, ‘This Old Man' is Agnell's reflection on life, starting ith what is...

10 ways to think creatively
What if what you want until you die can’t be done exactly as you imagined?
Consider it an opportunity for creative thinking.

Vial of LIFE
What is the Vial of LIFE Program It may sound like the fountain of youth, or miracle life-saver in a vial. It is neither. Instead, it’s information about your health care and wishes, stored in your fridge with a fridge sticker to announce its presence. LIFE stands for Lifesaving Information for Emergencies The Vial of LIFE sticker on your fridge alerts Emergency Response Teams (EMS) Paramedics and other health care providers who may come to your home
Connectivity and Cyber Seniors
Cyber Seniors: the growing internet demographic For the legion of cyber seniors, age 60-90 who rely on internet access to stay connected, it will come as no surprise that I put forward, in a recent tv panel, ‘internet for free’ for the elderly and low income as a...

Palliative Care: Doing ‘nothing’ is not an option
Dr Daphna Grossman wants to set the record straight “In healthcare it seems we talk about ‘doing everything’ or ‘doing nothing’. With Palliative care ‘nothing’ is not an option.
Medically Assisted Dying: the benefits of the process
When medical assistance in dying – MAID (also referred to as Medically Assisted Dying – MAD and Physician Assisted Dying – PAD ) was just a twinkle in eye in most of North America, I began my layman’s journey into learning all things end of life – encompassing much more than ‘help me die’. Now, with medical assistance in dying taking center stage, I’ve made it my business to attend every Town Hall, Presentation and Info session.

Taking Palliative Care Mainstream with the help of ePatients
Charlie Blotner, 21-year old ePatient and co-founder of the tweetchat for those with brain tumours #btsm. In learning more about Palliative Care, it just made sense that it should be part of standard services. Alas, not: If you’ve seen one #palliative care program, you’ve seen . . . one palliative care program – Jill Mendlen