Decision tool to help understand chances of dying after high risk surgery
“People worry about ‘dying poorly’, so one of the reasons for agreeing to surgery is the mistaken belief they’ll likely die – peacefully – in the Operating Room. This rarely happens.” Dr Gretchen Schwarze
To understand what can happen even if the surgery or operation is successful, Palliative doctor, Toby Campbell and Surgeon, Gretchen Schwarze feel stories are necessary to paint a picture for ‘consent’.
To illustrate, Dr Schwarze tells this story:
“She’s in her late 70’s, with chronic kidney failure and COPD. She’s making it a home with lots of support – but just barely. Now she has an aneurysm, that’s likely going to lead to a medical crisis. Should she have surgery for the aneurysm to prevent the medical crisis?”
Using statistics to describe success or failure, her family’s told:
- 50% chance of not surviving surgery
- 60% going to need dialysis for renal failure
- 80% chance going to need ventilator (breathing machine)
What the family hears is:
- 50% chance of survival
- 40% chance of NOT needing dialysis
- 20% chance of NOT needing
“So, they went for the surgery, took about 8 hours, overall doing well, as best as could be hoped for. When her family came to see her in the ICU, you can imagine what they saw. She was puffy with a breathing tube, with lines and wires and machines. They said, ‘this is not what she would have wanted’ and asked the team to withdraw all supports.”
We’ve been so good with innovating in so many areas, communication is not one of them.
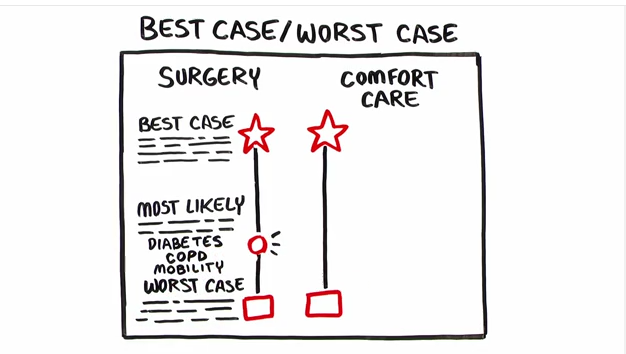
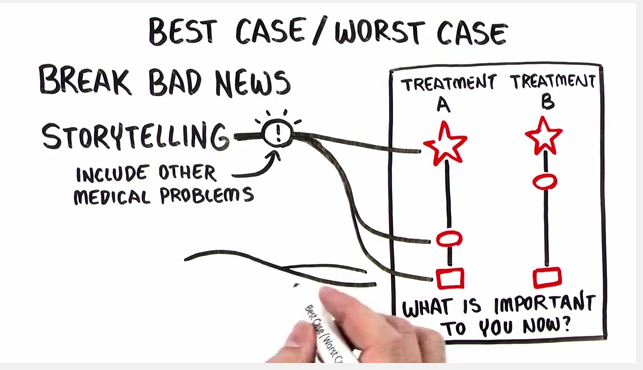
Drs Schwarze and Campbell are using a communication tool that walks patients and families through a best-case, worst-case and likely-case scenario – telling a story with each.
 In a 10-minute video to teach surgeons how to use this communication tool Dr Toby Campbell gives this patient as an example:
In a 10-minute video to teach surgeons how to use this communication tool Dr Toby Campbell gives this patient as an example:
‘Your patient is 81 years old, with fulminant c-difficile colitis (FCDC – is a highly lethal disease) He’s obese, and has end stage kidney disease (requiring a decision about dialysis). He has COPD (serious lung disease) and peritonitis (inflammation of the peritoneum — a silk-like membrane that lines your inner abdominal wall and covers the organs within your abdomen”
This patient is one sick man, whose family is now being asked about surgery to remove his colon. To help them understand about options – surgery or comfort care – Dr Campbell stresses, it’s important to ensure they know surgery won’t fix diabetes, COPD or improve his mobility.
Illustrating the patients journey opting for best case in comfort care, this picture tells the story that will end the same way – the patient dying – but more peacefully, with enough time for goodbye’s
Other than dying in the operating room, reasons for proceeding with surgery are complex.
- Repulsion of choosing one’s own death
- Not right ‘morally’ to choose ‘death’ over trying something
- Guilt: disappointing family or doctor
- Doctors are wrong about best case (the outcome is better than what the doctor has said)
- Miracles happen
To determine what to do, the question is not “What would he want?”
Rather,
“What would he say?
‘What’s important to you now”
“What are your hopes and expectations”
 However, Dr Schwarze in her presentation, High Stakes Surgical Decisions and Unwanted Care, points out medical realities:
However, Dr Schwarze in her presentation, High Stakes Surgical Decisions and Unwanted Care, points out medical realities:
- It takes more time to explain why surgery shouldn’t be done than to do the surgery
- Ethically conflicted about how to offer choices
- Expectation of referring doctors
- Clinical Momentum: all of the above plus a general drive towards facilitating treatment
Perhaps the Best/Worse/Most Likely communication tool, explained through stories, can help mitigate these issues, especially if the tool can be used early enough in the journey to help patients and families prepare for the outcomes of their decision.
One of the happy, unexpected results from using the tool, is that the it’s life of its own: Dr Schwarze followed up with patients and families 30 days after going through the Best Case Worst Case and found that many were using it to explain to other family and friends how the decision was made.
A new communication tool, spreading the old fashioned way: by word of mouth. To watch the 10 minute video: